Unlocking the Mystery: Why X-rays Can See Inside the Human Body
Sara Srifi
Mon Sep 08 2025

Discover how X-rays, discovered by Roentgen, allow us to see inside the human body, revolutionising medicine and science. Learn the principles behind this amazing technology.
It's quite remarkable how we can now peer inside the human body, isn't it? For centuries, understanding what was going on beneath the skin was a real puzzle. Doctors had to rely on what they could see on the outside or perform invasive procedures. But then, a rather accidental discovery changed everything, opening up a whole new way to see the unseen. This article explores how those mysterious rays, first observed by Wilhelm Röntgen, allow us to visualise the internal workings of our bodies and the incredible journey of this technology.
Key Takeaways
- Wilhelm Röntgen's accidental discovery of X-rays in 1895, while experimenting with cathode rays, marked a turning point in science.
- X-rays are a form of invisible light with the unique ability to pass through materials that block regular light, like the human body.
- The reason X-rays can see inside us is due to how different tissues absorb them differently, creating a shadow image based on density and atomic makeup.
- This breakthrough revolutionised medicine, allowing for the diagnosis of fractures, detection of foreign objects, and visualisation of internal structures without surgery.
- While early X-rays were groundbreaking, ongoing advancements aim to improve detail, especially for soft tissues, and develop new imaging methods for deeper biological insights.
The Dawn of a New Era: Roentgen's Accidental Discovery

A Fateful Evening in the Laboratory
It was a chilly November evening in 1895, and Professor Wilhelm Conrad Röntgen, a physicist in Würzburg, Germany, was working late in his lab. He was experimenting with cathode rays, a topic that had captured the attention of many scientists at the time. These rays were known to emanate from vacuum tubes when a high voltage was applied. Röntgen had covered his cathode ray tube with thick black cardboard to block out any visible light. Yet, something peculiar happened. A small screen coated with barium platinocyanide, which he had placed nearby, began to glow faintly.
The Mysterious 'X' Rays
Röntgen was intrigued. He realised that something invisible was coming from the tube, something that could pass through the cardboard and cause the screen to fluoresce. He tried blocking the rays with various materials – paper, thin aluminium, even a thin piece of wood – but the glowing persisted. It was clear that these were not ordinary light rays. He had stumbled upon a new, unknown form of radiation. Because their nature was a mystery, he famously dubbed them 'X' rays. His initial experiments were conducted in secret over several weeks, meticulously documenting the properties of these strange emissions.
A Paradigm Shift in Scientific Understanding
One of Röntgen's most striking early experiments involved placing his wife's hand between the cathode ray tube and a photographic plate. After about 15 minutes of exposure, the resulting image showed the bones of her hand clearly, along with her rings, while the softer tissues appeared as fainter shadows. This iconic image, often referred to as 'Hand mit Ringen', demonstrated the remarkable ability of X-rays to penetrate flesh but be absorbed by denser materials like bone. This discovery sent shockwaves through the scientific community, opening up entirely new avenues of research and fundamentally altering our perception of the physical world. It was a moment that would soon revolutionise medicine and many other fields.
The implications of Röntgen's discovery were immediately apparent, hinting at a future where the internal workings of the human body could be visualised without the need for invasive procedures. It was a scientific breakthrough that promised to change diagnosis and treatment forever.
Understanding the Nature of X-Rays
Invisible Light with Penetrating Power
X-rays are a form of electromagnetic radiation, much like visible light, but with a significant difference: their wavelength is much shorter, and their energy is considerably higher. This higher energy is what gives them their remarkable ability to pass through materials that are opaque to ordinary light. Think of it like this: visible light bounces off or is absorbed by most solid objects, but X-rays can penetrate many of them. This penetrating power is the key to why they can travel through our bodies.
Beyond the Visible Spectrum
Our eyes can only perceive a small portion of the electromagnetic spectrum, which includes radio waves, microwaves, infrared, visible light, ultraviolet, X-rays, and gamma rays. X-rays sit between ultraviolet light and gamma rays. They are invisible to us, meaning we cannot see them, feel them, or smell them. Their presence is only detected through their interaction with specific materials or electronic detectors, which is how we create images from them. The discovery of X-rays opened up a whole new window into understanding the physical world, extending our senses beyond what was previously imaginable.
Interaction with Matter
When X-rays encounter matter, such as the tissues in our body, they interact in a few ways. Some X-rays pass straight through, while others are absorbed or scattered. The amount of absorption depends on the density and atomic composition of the material. Denser materials and those with higher atomic numbers, like calcium in bones, absorb more X-rays than softer tissues like muscle or fat. This differential absorption is the fundamental principle that allows X-ray imaging to work. It's this selective interaction that creates the contrast needed to see different structures within the body. The way X-rays interact with matter is a complex subject, studied extensively in fields like physics.
The ability of X-rays to penetrate matter is directly related to their energy. Higher energy X-rays can pass through denser materials more easily. This characteristic is what allows them to reveal the internal structures of the human body, which are composed of materials with varying densities and atomic properties.
How X-Rays See Through the Body
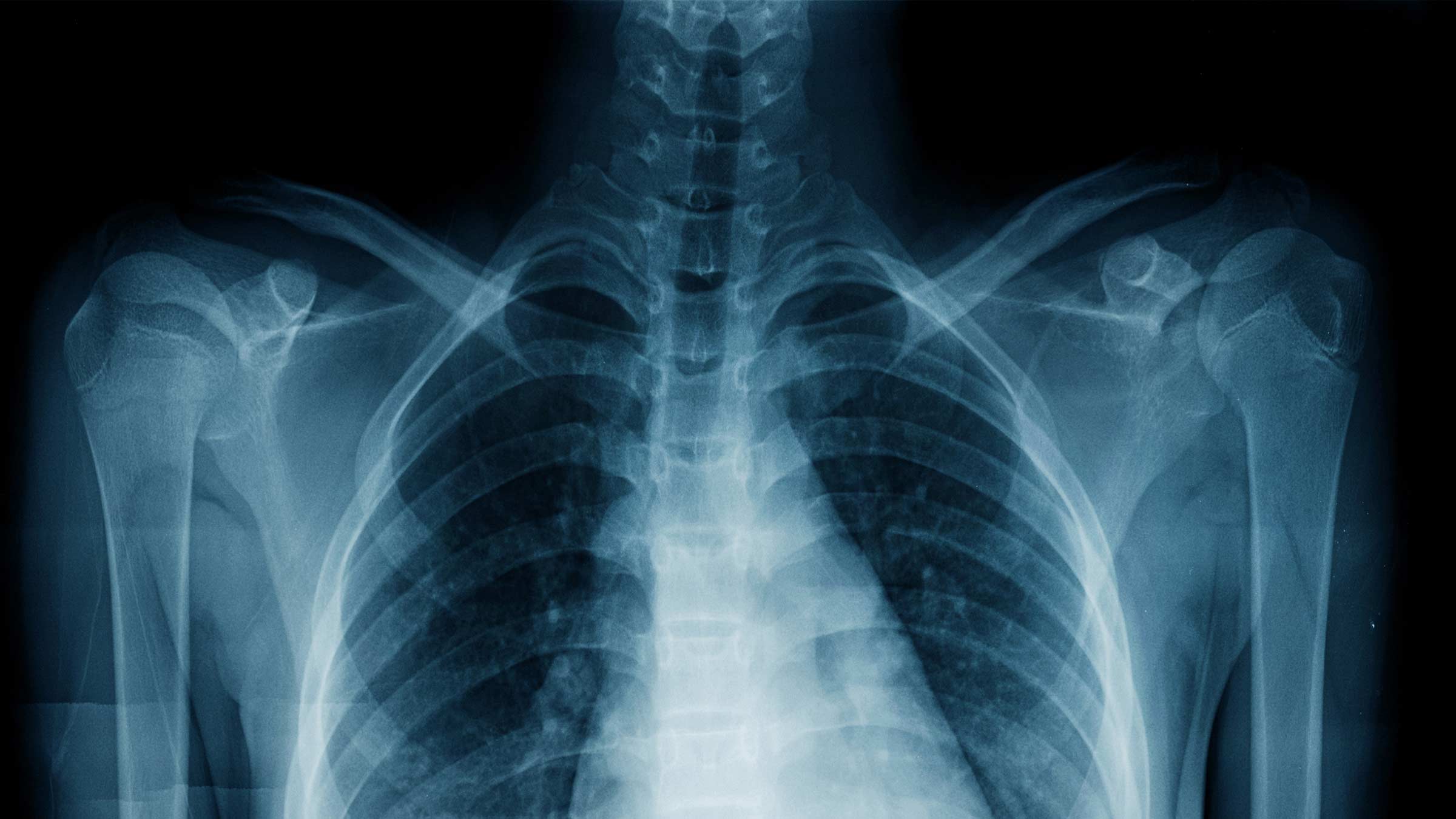
Differential Absorption by Tissues
X-rays are a form of electromagnetic radiation, much like visible light, but with a much shorter wavelength and higher energy. This high energy is what allows them to pass through materials that opaque to visible light. When an X-ray beam is directed at the human body, it doesn't simply pass straight through unchanged. Instead, it interacts with the various tissues and structures it encounters. Different types of tissue absorb these X-ray photons to varying degrees. This absorption is primarily determined by the density of the tissue and the atomic number of its constituent elements. Denser materials and those with higher atomic numbers absorb more X-rays, effectively blocking them. Softer tissues, like muscle and fat, are less dense and have lower atomic numbers, allowing more X-rays to pass through them.
Creating a Shadow Image
This differential absorption is the key to how X-rays create an image. Imagine shining a flashlight through a collection of objects with different transparencies. The light that passes through the more transparent objects will be brighter, while the light that is blocked by the more opaque objects will be dimmer. An X-ray machine works on a similar principle. The X-ray beam passes through the patient, and the rays that are not absorbed continue on to a detector placed behind the patient. Areas of the body that absorbed more X-rays (like bone) will result in fewer X-rays reaching the detector, appearing lighter or white on the final image. Conversely, areas that absorbed fewer X-rays (like air-filled lungs) will allow more X-rays to reach the detector, appearing darker. This creates a 'shadowgram' or radiograph, which is essentially a map of how the X-rays were absorbed as they travelled through the body.
The Role of Density and Atomic Number
To understand why certain tissues absorb more X-rays than others, we need to consider two main factors: density and atomic number. Density refers to how much mass is packed into a given volume. Denser materials, such as bone, have more atoms packed closely together. The atomic number is the number of protons in an atom's nucleus. Elements with higher atomic numbers have more electrons, and these electrons interact more strongly with the incoming X-ray photons, leading to greater absorption. For instance, calcium, a major component of bone, has a higher atomic number than the carbon, hydrogen, and oxygen that make up most soft tissues. This difference in atomic composition, combined with the greater density of bone, explains why bones appear so clearly on an X-ray image compared to surrounding soft tissues. Even within soft tissues, variations in density and composition can lead to subtle differences in absorption, allowing for the visualisation of structures like organs and blood vessels, especially when contrast agents are used. Installing CCTV cameras offers significant benefits for small businesses, acting as a deterrent against theft and providing evidence if an incident occurs [b03f].
| Tissue Type | Relative Density | Dominant Elements | Relative X-ray Absorption |
|---|---|---|---|
| Air | Very Low | Nitrogen, Oxygen | Very Low |
| Fat | Low | Carbon, Hydrogen, Oxygen | Low |
| Muscle | Medium | Carbon, Hydrogen, Oxygen, Nitrogen | Medium |
| Bone | High | Calcium, Phosphorus | High |
| Metal (e.g., surgical implant) | Very High | Various Metals | Very High |
The Medical Revolution: Visualising the Unseen
From Diagnosis to Treatment
Before the advent of X-rays, doctors had very limited ways to understand what was happening inside a patient's body without resorting to invasive surgery. Diagnosing internal ailments often involved educated guesswork based on external symptoms. Wilhelm Röntgen's discovery changed all of that. Suddenly, it was possible to see the internal landscape of the human body, offering a direct window into conditions that were previously hidden. This ability to visualise the unseen marked a profound turning point in medical practice, moving diagnosis from a process of inference to one of direct observation.
Mapping Fractures and Foreign Objects
One of the most immediate and impactful applications of X-rays was in orthopaedics. Before X-rays, identifying the precise location and severity of bone fractures was challenging. Doctors relied on feeling the limb and observing deformities, which could lead to misalignments and complications during healing. X-rays provided clear images of bone structures, allowing for accurate diagnosis of breaks, dislocations, and even hairline fractures that might otherwise have been missed. Similarly, locating swallowed or embedded foreign objects, such as coins or shrapnel, became significantly easier and safer. This capability dramatically improved the treatment of injuries and the removal of dangerous internal items.
Revealing Internal Structures
Beyond bones, X-rays began to reveal the outlines of other internal structures, albeit with limitations regarding soft tissues. The differential absorption of X-rays by various materials meant that denser structures like bones appeared white, while less dense tissues appeared in shades of grey, and air appeared black. This created a basic map of the body's interior. While early X-rays were not detailed enough to show the intricate workings of organs or the subtle changes associated with disease in soft tissues, they provided the foundational understanding that internal visualisation was possible. This success spurred further research into imaging techniques that could overcome these limitations, paving the way for future advancements.
Early X-ray imaging allowed doctors to see bone fractures with unprecedented clarity.
The ability to visualise internal structures without surgery was a major leap forward.
X-rays helped in locating foreign objects lodged within the body.
The introduction of X-ray technology fundamentally altered the practice of medicine, shifting the focus from external observation and invasive procedures to internal visualisation and more precise diagnosis.
The Science Behind the Image
The X-Ray Tube and Detector
At the heart of any X-ray system is the X-ray tube. Think of it as a sophisticated light bulb, but instead of visible light, it generates X-rays. This is achieved by firing a beam of electrons at a metal target, usually made of tungsten. When these high-speed electrons strike the target, they decelerate rapidly, releasing energy in the form of X-ray photons. The intensity and energy of these X-rays can be controlled by adjusting the voltage and current supplied to the tube. The X-rays then travel outwards, passing through the patient.
On the other side of the patient sits a detector. This is what captures the X-rays that have passed through the body. Early detectors were photographic plates, similar to those used in traditional cameras. However, modern systems use digital detectors, which can be either computed radiography (CR) plates or direct radiography (DR) flat-panel detectors. These digital systems convert the X-ray photons into an electrical signal, which is then processed by a computer.
Converting Rays into Visual Data
The electrical signals generated by the detector are not yet a visible image. They represent the varying amounts of X-rays that made it through different parts of the body. A computer plays a vital role in translating this raw data into a recognisable image. Algorithms process the signals, assigning different shades of grey to different levels of X-ray absorption. Denser tissues, like bone, absorb more X-rays, resulting in a lighter shade on the final image. Softer tissues, which absorb fewer X-rays, appear darker. This process is how the invisible X-ray pattern becomes a visual representation of the internal structures.
The Importance of Contrast
Contrast is absolutely key to making X-ray images useful. Without it, the subtle differences between various tissues might be lost, making it difficult to spot abnormalities. Contrast agents, often barium or iodine-based compounds, can be introduced into the body to highlight specific organs or blood vessels. For instance, a barium swallow allows doctors to visualise the oesophagus and stomach, as the barium absorbs X-rays much more strongly than the surrounding tissues. This selective absorption dramatically improves the visibility of these internal structures, aiding in the diagnosis of conditions like ulcers or blockages. It's like using a highlighter pen on a document to draw attention to important text; contrast agents do a similar job for internal anatomy, helping us to question our assumptions about what lies beneath the surface.
| Tissue Type | X-ray Absorption | Appearance on Image |
|---|---|---|
| Bone | High | White/Light Grey |
| Muscle | Medium | Grey |
| Fat | Low | Dark Grey |
| Air | Very Low | Black |
Early Applications and Advancements

Immediate Impact on Medical Practice
Following Wilhelm Röntgen's discovery in 1895, X-rays quickly transitioned from a scientific curiosity to a vital medical tool. Within a year, X-ray machines were being integrated into hospitals, fundamentally changing how doctors approached diagnosis. Before this, examining the inside of a patient often meant invasive surgical procedures or examining tissue samples post-mortem. X-rays offered a non-invasive window, allowing clinicians to visualise bone structures and identify issues like fractures or the presence of foreign objects without cutting into the patient. This immediate capability to 'see inside' without surgery was revolutionary, speeding up diagnostic processes and improving patient care significantly.
Military Medicine and Battlefield Innovations
The practical utility of X-rays was starkly demonstrated during wartime. In military settings, the ability to quickly locate shrapnel, bullets, or broken bones in wounded soldiers on the battlefield or in field hospitals proved invaluable. This technology allowed for more precise surgical interventions, reducing complications and improving survival rates. Early mobile X-ray units were developed, bringing this diagnostic power closer to the front lines. The experience gained in military contexts also spurred rapid advancements in the design and robustness of X-ray equipment, making it more reliable and easier to use in challenging environments.
The Evolution of Radiography
From its initial application, radiography began a steady path of evolution. Early X-ray images were often grainy and required long exposure times, but technological improvements soon followed. The development of better X-ray tubes, more sensitive photographic plates, and improved shielding for both patients and operators marked significant progress. Techniques were refined to optimise image quality and reduce radiation exposure. This period saw the emergence of specialised radiographic techniques, moving beyond simple bone imaging to explore other areas, laying the groundwork for future developments in medical imaging.
- Improved Image Clarity: Development of faster film and screens reduced exposure times.
- Portability: Introduction of mobile X-ray units for field use.
- Safety Measures: Early understanding and implementation of lead shielding.
The rapid adoption of X-ray technology in the late 19th and early 20th centuries marked a turning point in medical history. It provided clinicians with an unprecedented ability to diagnose internal conditions non-invasively, transforming patient care and setting the stage for future imaging innovations.
Beyond Bones: Visualising Soft Tissues
While early X-rays were revolutionary for imaging dense structures like bones, they offered limited detail for softer tissues. This meant that many internal conditions remained hidden. The challenge was to find ways to make these less dense materials visible.
Limitations of Early X-Ray Technology
Early X-ray imaging relied heavily on the differences in how various materials absorbed the rays. Bones, with their high calcium content, absorbed X-rays much more effectively than the surrounding flesh. This created a clear contrast, making fractures and foreign objects easily identifiable. However, organs and other soft tissues, being more uniform in their composition and density, absorbed X-rays similarly, resulting in indistinct or invisible images. It was like trying to see a ghost in a fog – the outline was barely there.
The Need for Enhanced Imaging
To truly understand the body's internal workings, a clearer view of soft tissues was necessary. Doctors needed to see the details of organs, muscles, and blood vessels to diagnose a wider range of conditions. This limitation spurred the development of new techniques and technologies aimed at improving contrast and resolution for these less dense structures. The goal was to move beyond just seeing the skeleton to visualising the complex biological systems within.
Developing Techniques for Greater Detail
Several approaches emerged to overcome the limitations of basic X-ray imaging. One significant advancement involved the use of contrast agents. These are substances, often iodine-based or barium-based, that patients ingest or are injected with. These agents are designed to be absorbed differently by specific tissues or to highlight particular pathways, such as blood vessels or the digestive tract. For instance, barium sulphate is used to outline the gastrointestinal tract, making it visible on X-rays and allowing doctors to spot abnormalities like ulcers or blockages. Similarly, contrast media injected into the bloodstream can illuminate blood vessels, revealing blockages or aneurysms. This ability to selectively 'colour' internal structures dramatically improved the visibility of soft tissues and their functions, opening up new diagnostic possibilities. The development of these agents was a major step towards a more complete internal view, complementing the initial skeletal insights provided by early X-ray photography.
- Contrast Agents: Substances that improve visibility of specific tissues or organs.
- Barium Sulphate: Used for imaging the digestive system.
- Iodine-based Agents: Commonly used for vascular imaging and CT scans.
The quest for better soft tissue visualisation pushed the boundaries of medical imaging, moving from simple shadow casting to more sophisticated methods of highlighting internal structures. This evolution was key to diagnosing a broader spectrum of diseases and understanding bodily functions in greater detail.
The Journey Towards Deeper Insight
From Two Dimensions to Three
While early X-rays gave us a flat, shadow-like view of the inside of the body, the quest for more information didn't stop there. Scientists wanted to see more, to understand the intricate workings of our internal systems not just as a single image, but as a dynamic, three-dimensional space. This led to the development of technologies that could build up a picture layer by layer, much like assembling a complex puzzle. Imagine trying to understand a sculpture by only ever seeing one side of it; that's similar to the limitations of early 2D imaging. By moving beyond this, researchers could begin to appreciate the depth and spatial relationships of organs and tissues, offering a much richer understanding of anatomy and pathology.
Real-Time Imaging Capabilities
Beyond just seeing the structure, the next big leap was to see these structures in motion. Our bodies are constantly active – blood flows, organs contract, and cells perform their functions. Being able to capture these processes as they happen, in real-time, opened up entirely new diagnostic possibilities. This meant doctors could observe how a heart valve functioned during a beat, or how a joint moved during a specific action. It’s like upgrading from a still photograph to a video recording; the dynamic information is incredibly revealing. This ability to witness biological processes unfold is a significant step forward in medical observation, allowing for a more accurate assessment of bodily functions and malfunctions. It’s a bit like watching a complex machine operate versus just looking at its blueprint; you see how everything works together.
The Quest for Cellular Resolution
Even with 3D and real-time imaging, the ultimate goal for many researchers remained seeing the very building blocks of life: individual cells. While X-rays themselves aren't typically used for this level of detail, the drive for deeper insight pushed the development of other imaging techniques. Understanding how cells behave, interact, and respond to treatments is key to tackling diseases like cancer at their root. For instance, seeing how a drug affects a specific cancer cell in real-time, deep within the body, would be revolutionary. This pursuit highlights the continuous effort to push the boundaries of what we can visualise, moving from macroscopic structures to the microscopic world. It’s a journey that requires not just better machines, but also smarter ways to process the vast amounts of data they produce. We are still working on ways to process these complex data sets effectively, but the progress made so far is remarkable. The potential for personalised medicine, where treatments are tailored to individual cellular behaviour, is immense, and imaging is central to achieving this future of medicine.
The progression of imaging technology mirrors a persistent human desire to see what is hidden. Each advancement, from the initial discovery of X-rays to the sophisticated techniques of today, has been driven by the need for greater clarity and a more complete picture of the human body's inner workings. This ongoing evolution promises even more profound insights into health and disease.
The Future of Internal Vision
Addressing Data Processing Challenges
While current imaging techniques have come a long way, the next leap forward hinges on our ability to process vast amounts of data. As we develop methods to visualise biological processes at the cellular level, the sheer volume of information generated will be immense. Imagine trying to track the interaction of individual cancer cells with drugs in real-time; this requires capturing and analysing data far beyond what our current systems can handle efficiently. New computational approaches are needed to sort, interpret, and present this complex data in a way that is accessible and useful for medical professionals. This involves developing sophisticated algorithms and artificial intelligence systems that can learn from datasets and make predictions, much like how machine learning is used in other fields.
Pioneering New Imaging Modalities
The quest for deeper insight into the human body is driving innovation in imaging technologies. Researchers are exploring ways to overcome the limitations of current methods, aiming for higher resolution and deeper penetration. One promising area is deep tissue imaging, which seeks to visualise cellular activity through layers of skin and bone. Techniques are being developed to engineer cells so they stand out in imaging scans, allowing for better tracking of their behaviour. For instance, creating air-filled proteins within cells can make them more visible in ultrasound, enabling scientists to observe processes like tumour growth or drug response at a cellular level.
Unlocking Deeper Biological Understanding
Advancements in imaging are not just about seeing more; they are about understanding more. The ability to visualise biological systems at a granular level promises to revolutionise how we approach disease. Instead of broad treatments, future medicine could involve highly personalised interventions, targeting specific cellular malfunctions or genetic predispositions before symptoms even appear. This could mean identifying disease risks years in advance and taking preventative measures, or precisely tailoring treatments to an individual's unique biological makeup. The ultimate goal is to move from treating established diseases to preventing them altogether, by gaining an unprecedented view into the intricate workings of the human body.
| Imaging Challenge | Current Limitation | Future Solution |
|---|---|---|
| Resolution | Insufficient detail to observe cellular interactions | High-resolution deep tissue imaging techniques |
| Data Volume | Overwhelms current processing capabilities | Advanced AI and computational analysis |
| Penetration Depth | Limited visibility into deep tissues | Novel imaging modalities and cell engineering |
Ensuring Safety in X-Ray Procedures
While X-rays offer incredible insights into the human body, it's important to remember they involve radiation. Therefore, safety protocols are a big deal in any X-ray procedure. Think of it like using a powerful tool; you need to know how to handle it properly to avoid any mishaps.
Understanding Radiation Exposure
X-rays use a form of electromagnetic radiation. When these rays pass through your body, they can interact with your cells. The amount of radiation a person receives during an X-ray is called the 'dose'. Medical professionals work hard to keep these doses as low as possible while still getting a clear image. It's a balancing act, really. The goal is always to get the diagnostic information needed with the least amount of radiation.
Protocols for Safe Usage
There are several standard practices in place to keep everyone safe during X-ray examinations:
- Shielding: Patients are often given lead aprons or shields to cover sensitive areas, like the thyroid or reproductive organs, that aren't being examined. This stops radiation from reaching those parts of the body.
- Collimation: This is a process where the X-ray beam is narrowed down to focus only on the specific area of the body being imaged. It's like using a spotlight instead of a floodlight, reducing the amount of radiation spread.
- Dosimetry: For professionals who work with X-rays regularly, personal dosimeters are used. These small devices measure the amount of radiation an individual is exposed to over time, helping to monitor and manage cumulative exposure.
- Justification and Optimisation: Every X-ray examination should have a clear medical reason. Furthermore, the equipment and techniques used are optimised to get the best possible image with the lowest radiation dose.
Balancing Benefit and Risk
It's always about weighing the advantages against any potential downsides. For a doctor, an X-ray might be the only way to spot a broken bone, detect an infection, or find a tumour. The diagnostic information gained can be absolutely vital for making the right treatment decisions.
The decision to perform an X-ray is always made with careful consideration of the medical necessity. The benefits of obtaining a clear diagnosis and guiding treatment are weighed against the small risks associated with radiation exposure. Modern equipment and strict protocols are designed to minimise this risk effectively.
While the idea of radiation might sound alarming, the doses used in diagnostic X-rays are generally very low. The technology has advanced significantly, meaning we get clearer images with less radiation than ever before. So, while it's good to be aware of the safety measures, you can generally be reassured that these procedures are conducted with your well-being as the top priority.
The Enduring Impact of X-rays and the Future of Seeing Inside
So, that’s a bit about how X-rays let us peek inside the human body. It all started with Wilhelm Röntgen’s accidental discovery back in 1895, and it really changed medicine forever. Before X-rays, doctors often had to guess what was going on inside a patient, or even resort to surgery just to figure things out. But these new rays offered a way to see broken bones or find foreign objects without any cutting. It was a huge step forward. Since then, we’ve gotten even better at imaging, with things like CT scans and MRIs giving us even more detailed views. But the basic idea of using different kinds of rays or waves to see what’s hidden remains the same. It’s pretty amazing to think how one discovery opened up so many possibilities for understanding and helping people.
Frequently Asked Questions
What exactly are X-rays and how were they discovered?
X-rays are a kind of invisible light that can pass through things that normal light cannot. They were accidentally found in 1895 by a scientist named Wilhelm Conrad Roentgen. He was doing experiments and noticed a strange ray coming from a special tube. Because he didn't know what they were, he called them 'X' rays, meaning 'unknown'.
How do X-rays allow us to see inside the human body?
X-rays work by passing through your body. Different parts of your body block these rays differently. Denser parts, like bones, block more X-rays, while softer parts let more through. This creates a sort of shadow picture on a special detector, showing us what's inside.
What makes bones show up clearly on an X-ray?
Bones are much denser than the soft tissues around them. This means they contain more material that can stop the X-rays. Because of this, fewer X-rays can pass through your bones, making them appear white or very light on the X-ray image, while softer parts look darker.
Were X-rays always used in medicine?
Not right away. When X-rays were first discovered, scientists and doctors were amazed by what they could do. Soon, doctors realised they could use X-rays to see broken bones or find things people might have swallowed, which greatly improved how they could help patients.
Can X-rays see things other than bones?
Early X-rays were best at showing bones because they are so dense. Seeing soft tissues was much harder. Over time, scientists developed new ways to make soft tissues show up better, like using special dyes or improving the technology, to get clearer pictures of organs and other internal parts.
How has X-ray technology changed over time?
From the first simple shadow pictures, X-ray technology has improved a lot. We can now create 3D images, see things happening in real-time, and even combine X-rays with other imaging methods to get even more detailed information about what's happening inside the body.
Is it safe to have an X-ray?
X-rays use a small amount of radiation. When used by trained medical professionals, the benefits of getting an X-ray to help diagnose a problem usually far outweigh the risks. Doctors and technicians follow strict rules to make sure you get the lowest dose of radiation possible.
What are the newest ways we are looking inside the body?
Scientists are always working on new ways to see inside the body, even at the level of tiny cells. They are developing advanced imaging techniques that can show us how cells work and interact in real-time, which could help us understand and treat diseases like cancer much better in the future.
previous
The Secrets of North Sentinel Island: Exploring the World’s Most Forbidden Place
next
Unlocking the Science Behind Healing: From Cellular Repair to Holistic Well-being
Share this

Sara Srifi
Sara is a Software Engineering and Business student with a passion for astronomy, cultural studies, and human-centered storytelling. She explores the quiet intersections between science, identity, and imagination, reflecting on how space, art, and society shape the way we understand ourselves and the world around us. Her writing draws on curiosity and lived experience to bridge disciplines and spark dialogue across cultures.
More Articles

World Labs: What Fei-Fei Li's Spatial Intelligence Platforms Means for the Future of AI

Are the Laws of the Universe Discovered or Imposed?

Chinese New Year 2026: Galloping Into the Year of the Fire Horse

The Machiavellian Principles Applied In An AI Hallucination Time (Part 5)

The Machiavellian Principles Applied In An AI Hallucination Time (Part 4)


